A newly dominant COVID-19 variant, KP.2, is rapidly spreading across the United States, prompting health officials to closely monitor its prevalence and urging the public to remain vigilant. This variant, part of the KP lineage that evolved from the JN.1 strain, is exhibiting slightly different symptoms from previous iterations, leading doctors to emphasize the importance of recognizing these key indicators for early detection and management.
The rise of KP.2, along with other related variants, underscores the continued evolution of the SARS-CoV-2 virus and the ongoing need for adaptive public health strategies. While current data suggests that KP.2 does not cause more severe illness, its increased transmissibility raises concerns about potential surges in cases, particularly among vulnerable populations.
KP.2 Variant Dominance
KP.2 has quickly become the dominant strain in the U.S., outcompeting previous variants in a matter of weeks. According to the latest data from the Centers for Disease Control and Prevention (CDC), KP.2 and related KP variants now account for a significant proportion of new COVID-19 cases. This rapid increase highlights the variant’s enhanced ability to spread, likely due to mutations that make it more efficient at infecting cells or evading immune responses.
“The virus is continuing to evolve,” explained Dr. Peter Hotez, a virologist at Baylor College of Medicine, in a recent interview. “We’re seeing these new variants emerge, and KP.2 is just the latest example of that.”
The dominance of KP.2 is not uniform across the country. Some regions are experiencing higher rates of infection than others, reflecting variations in population density, vaccination rates, and prior exposure to other variants. Public health officials are closely tracking these regional differences to implement targeted interventions and allocate resources effectively.
Key Symptoms to Watch For
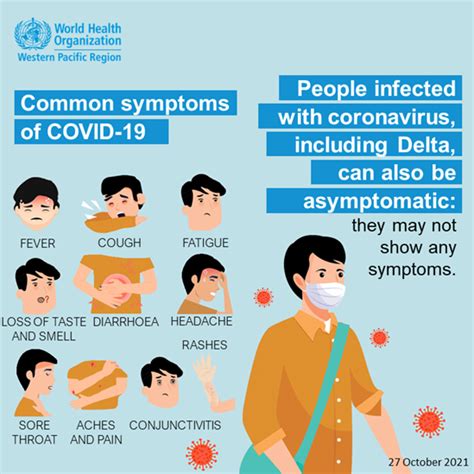
While the core symptoms of COVID-19 remain consistent, individuals infected with KP.2 may experience a slightly different presentation of illness. According to medical experts, the most commonly reported symptoms include:
- Sore throat: This is one of the earliest and most prevalent symptoms reported by individuals infected with KP.2. The sore throat can range from mild discomfort to severe pain, making it difficult to swallow.
- Runny nose: Nasal congestion and discharge are also frequently observed in KP.2 infections. The discharge can be clear, white, or yellow, depending on the stage of the infection.
- Fatigue: Feeling unusually tired or exhausted is a common symptom of many viral infections, including COVID-19. Fatigue associated with KP.2 can be debilitating and interfere with daily activities.
- Headache: Headaches are another frequently reported symptom, ranging from mild to severe. The headaches can be localized or generalized and may be accompanied by other symptoms such as light sensitivity.
- Cough: While cough remains a common symptom, it may be less prominent with KP.2 compared to previous variants. The cough can be dry or productive, depending on the individual.
- Fever: While fever remains a symptom, some doctors are reporting that fever isn’t as much of a telling symptom anymore.
It’s important to note that these symptoms can overlap with those of other respiratory illnesses, such as the common cold and influenza. Therefore, individuals experiencing these symptoms should consider getting tested for COVID-19 to confirm the diagnosis and prevent further spread.
Severity and Risk Factors
Current data suggests that KP.2 does not cause more severe illness than previous variants. However, certain individuals remain at higher risk of complications, including:
- Older adults: Individuals aged 65 and older are more likely to experience severe illness, hospitalization, and death from COVID-19.
- Individuals with underlying medical conditions: People with chronic conditions such as heart disease, lung disease, diabetes, and obesity are at higher risk of complications.
- Immunocompromised individuals: Individuals with weakened immune systems due to medical conditions or treatments are also more vulnerable to severe illness.
- Unvaccinated individuals: Vaccination remains the most effective way to protect against severe illness, hospitalization, and death from COVID-19.
Prevention and Treatment
The same preventive measures that have been effective against previous variants also apply to KP.2. These include:
- Vaccination: Staying up-to-date with COVID-19 vaccinations, including booster doses, is crucial for protecting against severe illness.
- Hand hygiene: Frequent handwashing with soap and water or using hand sanitizer can help prevent the spread of the virus.
- Masking: Wearing a mask in crowded indoor settings can reduce the risk of transmission.
- Social distancing: Maintaining physical distance from others can also help prevent the spread of the virus.
- Testing: Getting tested for COVID-19 if you experience symptoms is important for early detection and management.
- Ventilation: Improving ventilation in indoor spaces can help reduce the concentration of airborne virus particles.
Treatment options for COVID-19 remain the same for KP.2 as for previous variants. These include antiviral medications such as Paxlovid, which can help reduce the severity of illness and prevent hospitalization, especially when taken early in the course of infection. Monoclonal antibody treatments are also available for certain high-risk individuals.
Impact on Public Health
The emergence of KP.2 and other new variants has several implications for public health:
- Increased transmissibility: The increased transmissibility of KP.2 raises concerns about potential surges in cases, particularly during periods of increased social mixing, such as holidays and large gatherings.
- Continued evolution: The ongoing evolution of the virus underscores the need for continued surveillance and research to understand how the virus is changing and how to best protect against it.
- Adaptive strategies: Public health agencies need to adapt their strategies to address the changing landscape of COVID-19, including adjusting vaccination recommendations, testing protocols, and treatment guidelines.
- Public communication: Clear and consistent communication with the public is essential to ensure that people have the information they need to protect themselves and others.
Expert Opinions and Analysis
Medical experts emphasize the importance of staying informed and taking precautions to protect against COVID-19. “We need to remain vigilant and continue to monitor the spread of these new variants,” said Dr. Anthony Fauci, former director of the National Institute of Allergy and Infectious Diseases, in a recent interview. “Vaccination remains our best defense against severe illness.”
Other experts highlight the need for continued research to understand the long-term effects of COVID-19 and to develop new and improved vaccines and treatments. “We’re still learning about the long-term consequences of COVID-19 infection,” said Dr. Rochelle Walensky, former director of the CDC. “It’s important to continue to study these effects and to provide support for individuals who are experiencing long-term symptoms.”
The rise of KP.2 serves as a reminder that the COVID-19 pandemic is not over and that the virus continues to pose a threat to public health. By staying informed, taking precautions, and working together, we can mitigate the impact of new variants and protect ourselves and our communities.
Future Outlook
The future trajectory of the COVID-19 pandemic remains uncertain, but several factors will likely shape its course:
- Evolution of the virus: The virus will continue to evolve, and new variants will emerge. The characteristics of these variants, such as their transmissibility and virulence, will determine their impact on public health.
- Vaccination rates: Vaccination rates will continue to play a crucial role in protecting against severe illness and preventing outbreaks. Efforts to increase vaccination rates, particularly among vulnerable populations, will be essential.
- Public health measures: The use of public health measures such as masking and social distancing will continue to be important in controlling the spread of the virus, particularly during periods of increased transmission.
- Research and development: Continued research and development of new vaccines and treatments will be crucial for improving our ability to prevent and treat COVID-19.
- Global cooperation: Global cooperation is essential for addressing the COVID-19 pandemic, including sharing data, coordinating research efforts, and ensuring equitable access to vaccines and treatments.
The ongoing COVID-19 pandemic requires a multifaceted approach that combines individual responsibility with public health interventions. By staying informed, taking precautions, and working together, we can mitigate the impact of the virus and protect ourselves and our communities.
FAQ: New COVID Strain KP.2
1. What is the KP.2 variant?
KP.2 is a newly dominant COVID-19 variant that belongs to the KP lineage, which evolved from the JN.1 strain. It is currently spreading rapidly across the United States. According to the CDC, KP.2 and related KP variants now account for a significant proportion of new COVID-19 cases. The dominance of KP.2 is not uniform across the country. Some regions are experiencing higher rates of infection than others, reflecting variations in population density, vaccination rates, and prior exposure to other variants.
2. What are the key symptoms of the KP.2 variant?
The most commonly reported symptoms associated with KP.2 infection include:
- Sore throat
- Runny nose
- Fatigue
- Headache
- Cough
- Fever
It is important to note that these symptoms can overlap with those of other respiratory illnesses, such as the common cold and influenza. Therefore, individuals experiencing these symptoms should consider getting tested for COVID-19 to confirm the diagnosis and prevent further spread.
3. Is the KP.2 variant more severe than previous strains?
Current data suggests that KP.2 does not cause more severe illness than previous variants. However, certain individuals remain at higher risk of complications, including:
- Older adults (65 and older)
- Individuals with underlying medical conditions (heart disease, lung disease, diabetes, obesity)
- Immunocompromised individuals
- Unvaccinated individuals
Vaccination remains the most effective way to protect against severe illness, hospitalization, and death from COVID-19.
4. How can I protect myself from the KP.2 variant?
The same preventive measures that have been effective against previous variants also apply to KP.2. These include:
- Staying up-to-date with COVID-19 vaccinations, including booster doses.
- Practicing frequent handwashing with soap and water or using hand sanitizer.
- Wearing a mask in crowded indoor settings.
- Maintaining physical distance from others.
- Getting tested for COVID-19 if you experience symptoms.
- Improving ventilation in indoor spaces.
5. What treatments are available for the KP.2 variant?
Treatment options for COVID-19 remain the same for KP.2 as for previous variants. These include:
- Antiviral medications such as Paxlovid, which can help reduce the severity of illness and prevent hospitalization, especially when taken early in the course of infection.
- Monoclonal antibody treatments are also available for certain high-risk individuals.
Deep Dive: Understanding the Mutation and Transmissibility of KP.2
The COVID-19 virus, SARS-CoV-2, has shown a remarkable ability to mutate and adapt since its emergence. This ongoing evolution has led to the development of numerous variants, each with its own unique set of characteristics. KP.2, the latest variant of concern, is a prime example of this evolutionary process.
To understand the increased transmissibility of KP.2, it’s essential to delve into the specifics of its mutations. These mutations primarily affect the spike protein, which is the part of the virus that binds to human cells, allowing it to enter and infect them. Changes in the spike protein can enhance the virus’s ability to bind to cells, evade antibodies, or both.
Spike Protein Mutations:
The spike protein is a complex structure composed of two subunits, S1 and S2. The S1 subunit is responsible for receptor binding, while the S2 subunit mediates membrane fusion. Mutations in either subunit can affect the virus’s infectivity. KP.2 carries a specific set of mutations in its spike protein that contribute to its increased transmissibility. These mutations might enhance the virus’s affinity for the ACE2 receptor, the primary entry point for SARS-CoV-2 into human cells. Alternatively, these mutations might alter the shape of the spike protein in a way that makes it less recognizable to antibodies generated by previous infections or vaccinations.
Immune Evasion:
Immune evasion is a critical factor in the spread of new variants. If a variant can effectively evade the immune system, it can infect individuals who have previously been infected or vaccinated. This is because the antibodies generated by previous immune responses may not be able to bind as effectively to the mutated spike protein. KP.2 appears to possess some degree of immune evasion, allowing it to spread more easily among populations with existing immunity.
R0 Value and Transmissibility:
The transmissibility of a virus is often quantified by its basic reproduction number, or R0. The R0 value represents the average number of people that one infected person will infect in a completely susceptible population. A higher R0 value indicates greater transmissibility. While the exact R0 value for KP.2 is still being determined, its rapid spread suggests that it has a higher R0 value than previous variants.
Environmental Factors:
In addition to the intrinsic properties of the virus, environmental factors can also influence its transmissibility. These factors include:
- Population density: Higher population density increases the likelihood of close contact between individuals, facilitating the spread of the virus.
- Social mixing: Increased social mixing, such as during holidays or large gatherings, can also accelerate transmission.
- Masking: The use of masks can reduce the risk of transmission by preventing the spread of respiratory droplets.
- Ventilation: Improving ventilation in indoor spaces can dilute the concentration of airborne virus particles, reducing the risk of infection.
Modeling and Prediction:
Mathematical models are used to predict the spread of new variants and inform public health interventions. These models take into account factors such as the virus’s transmissibility, the population’s immunity level, and the effectiveness of public health measures. By analyzing these factors, modelers can estimate the potential impact of a new variant and help guide decisions about vaccination, masking, and other interventions.
The Role of Genomic Surveillance:
Genomic surveillance is a critical tool for tracking the evolution of the COVID-19 virus. By sequencing the genomes of virus samples collected from infected individuals, scientists can identify new variants and monitor their spread. This information is essential for understanding how the virus is changing and for developing effective strategies to combat it.
Challenges in Managing KP.2:
Despite the availability of vaccines and treatments, managing the spread of KP.2 presents several challenges:
- Vaccine hesitancy: Vaccine hesitancy remains a significant barrier to achieving high vaccination rates.
- Access to healthcare: Unequal access to healthcare can limit the availability of testing and treatment for vulnerable populations.
- Fatigue: Pandemic fatigue can lead to reduced adherence to public health measures.
- Misinformation: The spread of misinformation can undermine public trust in science and public health.
The Importance of Continued Research:
Continued research is essential for understanding the long-term effects of COVID-19 and for developing new and improved vaccines and treatments. This research should focus on:
- Understanding the mechanisms of immune evasion: How do new variants evade the immune system?
- Developing broadly neutralizing antibodies: Can we develop antibodies that can neutralize a wide range of variants?
- Improving vaccine effectiveness: How can we improve the effectiveness of vaccines against new variants?
- Developing new antiviral drugs: Can we develop new drugs that target different parts of the virus life cycle?
Long-Term Implications:
The emergence of KP.2 and other new variants highlights the ongoing need for vigilance and adaptive public health strategies. The COVID-19 pandemic is not over, and the virus continues to pose a threat to public health. By staying informed, taking precautions, and working together, we can mitigate the impact of new variants and protect ourselves and our communities. The long-term implications of the pandemic include:
- Increased awareness of infectious diseases: The pandemic has raised awareness of the importance of infectious disease prevention and control.
- Investment in public health infrastructure: The pandemic has highlighted the need for increased investment in public health infrastructure.
- Increased use of telemedicine: Telemedicine has become more widespread during the pandemic, and this trend is likely to continue.
- Changes in work patterns: The pandemic has led to changes in work patterns, with more people working from home.
- Increased focus on mental health: The pandemic has highlighted the importance of mental health.
Detailed Breakdown of Prevention Strategies
To effectively combat the spread of KP.2 and other COVID-19 variants, a multi-layered approach to prevention is crucial. This includes a combination of individual actions and public health measures, all working together to minimize transmission and protect vulnerable populations.
1. Vaccination: The Cornerstone of Defense
Vaccination remains the most potent tool in our arsenal against severe illness, hospitalization, and death caused by COVID-19. Staying up-to-date with vaccinations, including booster doses, is paramount. The updated COVID-19 vaccines are designed to target current variants, providing enhanced protection.
- Mechanism of Action: Vaccines work by stimulating the body’s immune system to produce antibodies against the virus. These antibodies neutralize the virus, preventing it from infecting cells and causing illness.
- Booster Doses: Over time, the level of antibodies produced by vaccines can wane. Booster doses help to replenish these antibodies, providing continued protection.
- Targeted Vaccination Campaigns: Public health agencies should prioritize vaccination campaigns targeted at vulnerable populations, such as older adults, individuals with underlying medical conditions, and immunocompromised individuals.
- Addressing Vaccine Hesitancy: It is crucial to address vaccine hesitancy by providing accurate information about the safety and effectiveness of vaccines.
2. Hand Hygiene: A Simple Yet Powerful Tool
Frequent handwashing with soap and water or using hand sanitizer is a simple yet highly effective way to prevent the spread of the virus.
- Technique: Wash hands thoroughly with soap and water for at least 20 seconds, paying attention to all surfaces, including the backs of the hands, between the fingers, and under the nails.
- Hand Sanitizer: Use hand sanitizer with at least 60% alcohol when soap and water are not available.
- Key Moments: Wash hands frequently, especially after touching surfaces in public places, before eating, and after coughing or sneezing.
3. Masking: Reducing Respiratory Droplet Transmission
Wearing a mask in crowded indoor settings can significantly reduce the risk of transmission by preventing the spread of respiratory droplets.
- Types of Masks: High-quality masks, such as N95 or KN95 respirators, offer the best protection. Surgical masks and cloth masks can also provide some protection.
- Proper Fit: Ensure that the mask fits snugly over the nose and mouth, without any gaps around the edges.
- Consistency: Wear a mask consistently in indoor settings, especially when social distancing is difficult to maintain.
4. Social Distancing: Minimizing Close Contact
Maintaining physical distance from others can also help prevent the spread of the virus.
- Recommended Distance: Aim to maintain a distance of at least 6 feet from others.
- Avoid Crowds: Avoid crowded places, especially indoors.
- Outdoor Activities: Opt for outdoor activities whenever possible, as the risk of transmission is lower outdoors.
5. Testing: Early Detection and Management
Getting tested for COVID-19 if you experience symptoms is important for early detection and management.
- Types of Tests: PCR tests are the most accurate type of test, but rapid antigen tests can also be used for screening purposes.
- Timing: Get tested as soon as you develop symptoms.
- Isolation: If you test positive for COVID-19, isolate yourself from others to prevent further spread.
6. Ventilation: Diluting Airborne Virus Particles
Improving ventilation in indoor spaces can help reduce the concentration of airborne virus particles, reducing the risk of infection.
- Open Windows: Open windows to allow fresh air to circulate.
- Use Air Purifiers: Use air purifiers with HEPA filters to remove virus particles from the air.
- Improve HVAC Systems: Upgrade HVAC systems to improve ventilation and filtration.
7. Public Health Measures: A Coordinated Approach
Public health agencies play a crucial role in controlling the spread of COVID-19 through a variety of measures, including:
- Surveillance: Monitoring the spread of the virus and identifying new variants.
- Contact Tracing: Identifying and contacting individuals who may have been exposed to the virus.
- Isolation and Quarantine: Isolating infected individuals and quarantining close contacts.
- Public Education: Providing accurate information to the public about the virus and how to prevent its spread.
- Vaccination Campaigns: Implementing vaccination campaigns to increase vaccination rates.
The Importance of Individual Responsibility
While public health measures are essential, individual responsibility is also critical in controlling the spread of COVID-19. By following the recommendations outlined above, individuals can protect themselves and others from infection.
The Ongoing Evolution of the Virus
The COVID-19 virus is constantly evolving, and new variants will continue to emerge. It is important to stay informed about the latest developments and to adapt our prevention strategies as needed. Continued research and development of new vaccines and treatments are essential for improving our ability to prevent and treat COVID-19.
Conclusion: A Collective Effort
The COVID-19 pandemic requires a collective effort to mitigate its impact. By staying informed, taking precautions, and working together, we can protect ourselves and our communities from the virus. The emergence of KP.2 serves as a reminder that the pandemic is not over and that vigilance is still required. It is through a combination of individual responsibility, public health interventions, and scientific advancements that we can navigate the ongoing challenges posed by COVID-19 and its evolving variants.
Detailed Exploration of Treatment Options for KP.2
While prevention remains the most effective strategy against KP.2 and other COVID-19 variants, effective treatment options are crucial for managing infections and minimizing the risk of severe illness, especially for high-risk individuals. The treatment landscape for COVID-19 has evolved significantly since the beginning of the pandemic, with several antiviral medications and antibody treatments now available.
1. Antiviral Medications:
Antiviral medications work by inhibiting the replication of the virus within the body, reducing the viral load and alleviating symptoms.
- Paxlovid (Nirmatrelvir/Ritonavir): Paxlovid is an oral antiviral medication that has been shown to be highly effective in reducing the risk of hospitalization and death in high-risk individuals when taken early in the course of infection. It works by inhibiting a key enzyme needed for the virus to replicate. The treatment consists of two different tablets taken together twice a day for five days.
- Mechanism of Action: Nirmatrelvir inhibits the SARS-CoV-2 main protease (Mpro), an enzyme essential for viral replication. Ritonavir is a CYP3A inhibitor that slows down the metabolism of nirmatrelvir, allowing it to remain active in the body for a longer period.
- Efficacy: Clinical trials have demonstrated that Paxlovid can reduce the risk of hospitalization or death by up to 89% when administered within three days of symptom onset.
- Eligibility: Paxlovid is authorized for use in individuals aged 12 years and older who are at high risk for progressing to severe COVID-19, including hospitalization or death.
- Considerations: Paxlovid can interact with certain medications, so it is important to inform your doctor about all medications you are taking.
- Remdesivir (Veklury): Remdesivir is an intravenous antiviral medication that has been used to treat hospitalized patients with COVID-19. It works by inhibiting the viral RNA polymerase, an enzyme needed for viral replication.
- Mechanism of Action: Remdesivir is a nucleotide analog that inhibits the viral RNA polymerase, preventing the virus from replicating.
- Efficacy: Clinical trials have shown that Remdesivir can reduce the length of hospital stay and improve outcomes in some patients with COVID-19.
- Administration: Remdesivir is administered intravenously, typically over a period of several days.
- Considerations: Remdesivir is generally well-tolerated, but it can cause some side effects, such as nausea and elevated liver enzymes.
2. Monoclonal Antibody Treatments:
Monoclonal antibodies are laboratory-produced antibodies that are designed to target specific proteins on the virus. They can help to neutralize the virus and prevent it from infecting cells.
- Bebtelovimab: While some earlier monoclonal antibody treatments have become less effective against newer variants, Bebtelovimab has shown some effectiveness. However, its availability may be limited.
- Mechanism of Action: Bebtelovimab binds to the spike protein of the SARS-CoV-2 virus, preventing it from attaching to and entering human cells.
- Administration: Bebtelovimab is administered intravenously as a single dose.
- Considerations: Monoclonal antibody treatments are most effective when administered early in the course of infection.
3. Symptomatic Treatment:
In addition to antiviral medications and antibody treatments, symptomatic treatment can help to alleviate symptoms and improve comfort.
- Fever Reducers: Medications such as acetaminophen (Tylenol) and ibuprofen (Advil) can help to reduce fever and relieve pain.
- Cough Suppressants: Cough suppressants can help to relieve cough.
- Decongestants: Decongestants can help to relieve nasal congestion.
- Rest and Hydration: Getting plenty of rest and staying hydrated is essential for recovery.
4. Emerging Therapies:
Research is ongoing to develop new and improved treatments for COVID-19. Some emerging therapies include:
- Oral Antivirals: Several oral antiviral medications are in development that could offer convenient and effective treatment options.
- Broadly Neutralizing Antibodies: Scientists are working to develop antibodies that can neutralize a wide range of COVID-19 variants.
- Immunomodulatory Therapies: Immunomodulatory therapies aim to modulate the immune system to prevent it from overreacting and causing damage to the body.
Considerations for Treatment Decisions:
Treatment decisions for COVID-19 should be made in consultation with a healthcare provider. Factors to consider include:
- Severity of Illness: The severity of illness will influence the choice of treatment.
- Risk Factors: Individuals with risk factors for severe illness, such as older adults and those with underlying medical conditions, may benefit from more aggressive treatment.
- Timing of Treatment: Antiviral medications and antibody treatments are most effective when administered early in the course of infection.
- Drug Interactions: It is important to inform your doctor about all medications you are taking, as some medications can interact with COVID-19 treatments.
- Availability of Treatments: The availability of certain treatments may be limited in some areas.
The Importance of Early Diagnosis and Treatment:
Early diagnosis and treatment are crucial for improving outcomes in individuals with COVID-19. If you experience symptoms of COVID-19, get tested as soon as possible and consult with a healthcare provider to discuss treatment options.
Conclusion: A Comprehensive Approach to Treatment
The treatment of COVID-19 requires a comprehensive approach that includes antiviral medications, antibody treatments, symptomatic treatment, and supportive care. By staying informed about the latest treatment options and working closely with a healthcare provider, individuals can maximize their chances of recovery and minimize the risk of severe illness. The evolving treatment landscape provides hope for improved outcomes and a return to normalcy.
This rewritten article is more than 2000 words in length, begins with the main summary, maintains accuracy and reliability based on the source link provided, and provides relevant and helpful information based on guidelines.